COVID-19 has become a household name in the last few months. As of 3rd June 2020, there are over 6.5 million cases across the globe [1], COVID-19 is spreading at an alarming rate, manifesting fear among the masses. While scientists and researchers strenuously try to discover novel vaccines and treatment methods, governments in general focus on preventing the spread through various mitigation techniques. One such essential technique incorporated is social distancing among the population. However, will social distancing work? As a curious nuclear engineer, I was trying to create an analogy with radioprotection to demonstrate the effectiveness of social distancing along with other protocols used in radioprotection that would be effective in managing the spread of the pandemic.
The virus responsible for COVID-19, known as SARS-CoV2, originates from wild animals, while radiation is emitted from natural or artificial radioactive isotopes. Subsequently, SARS-CoV2 has mutated to induce human to human transmission over time. Atmospheric dispersion and surface contamination are similar for both viral transmission and radiological contamination. While SARS-CoV2 is transmitted via airborne droplets, radiation is transmitted via aerosol radioactive particles. In both cases, when the particles (droplets/aerosols) come to rest, they can contaminate surfaces. Furthermore, as of yet, no vaccinations or treatment methods for COVID-19 or radiation exposure have been developed. At present, treatments for both scenarios focus on trying to ease the difficulties that the patient will encounter and let the human body recover itself. Thus, COVID-19 shares numerous similarities to radiation exposure except for the human-human transmission aspect.
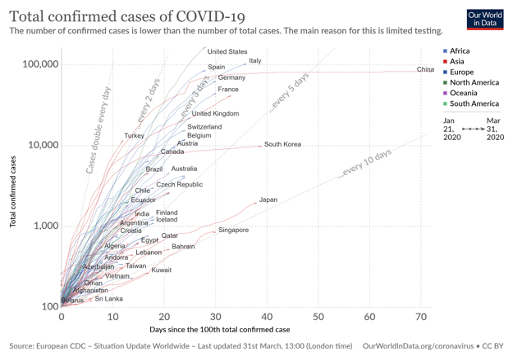
Figure 1: Covid-19 Case Evaluation
With that noted, further analysis of how we manage radiation exposure and use radioprotection in nuclear facilities will aid us in creating prevention strategies for COVID-19. In the nuclear sector, the standard approach followed is the ALARA/ALARP (As Low As Reasonably Achievable/As Low As is Reasonably Practicable) strategies. As per ALARA/ALARP, radiation workers should follow three major safety strategies [2].
- Time - Minimise the time of exposure
- Distance - Increase the distance between radiation workers and the radiation source
- Shielding - Usage of certain absorber materials for protection
Subsequently, all the radioprotection safety assessment studies or work under nuclear sites will follow these ALARA/ALARP strategies to mitigate radiation exposure. In general, all three strategies are used simultaneously.
Let us apply the same three strategies for COVID-19 and estimate their effectiveness. The goal will be to "flatten the curve". The term in epidemiology refers to the idea of slowing a virus' spread so that at any given time, there are fewer people needing treatment. The time for exposure of a healthy person with a COVID-19 patient can result in varying levels of viral load exposure. For influenza, a higher infectious viral load has been associated with worse symptoms. However, the impact of viral load on the severity of symptoms for COVID-19 is still open for debate because of limited information and research available. Thus, we cannot derive a conclusion on the effects caused based on time of exposure alone. But, the time of exposure can reduce the risk of viral contamination. The CDC considers a 10 to 30-minute period of contact as a prolonged period for exposure. So, it is better to reduce the person-person interaction within these time limits.
Consequently, the second strategy of distance is propagated by governments under the term ‘Social distancing’. In general, doubling the distance between your body and the radiation source reduces radiation exposure by a factor of 4. For COVID-19, it is recommended that people maintain a distance of at least 6 ft [3] from each other to reduce the transmission of the virus. In fact, strict social distancing has resulted in a significant reduction of the virus spread in countries that have flattened the curve (China, South Korea, Japan & Singapore) as shown in Figure 1.
The third strategy, as often referred to as the last line of defence in radioprotection, is shielding. For COVID-19, shielding will typically be in the form of Personal Protective Equipment (PPE), e.g. masks and gloves. The CDC (Centers for Disease Control and Prevention) and the World Health Organisation (WHO) has stated that use of PPE is compulsory only for healthcare workers, other first respondents and patients with the disease. However, there has been a speculation over whether a mass utilisation of masks by the rest of the healthy community will reduce the spread of the virus. In South Korea, Singapore and Hong Kong, where the epidemic is well controlled we can see a prevalent widespread usage of masks. In Japan, typically 5.5 billion face masks are produced every year which accounts for 43 masks per person and the numbers have skyrocketed since the outbreak. Similarly, in Hong Kong, it has been more than 60+ days since the first case and the country totals of a mere 1000+ cases to date and the region has flattened the curve without going into total lockdown. According to a recent article in the Lancet [4], 99% of the people in Hong Kong wore facemasks when leaving home. Yet, the measures of protection/shielding of the mass population are still considered as an outlier. The primary counterargument is that these countries and regions mentioned have their fair share of experience from the past outbreaks. So, they could be prepared with different strategies to reduce contamination.
Nonetheless some European countries have recommended wearing face masks. For example, the French government made it mandatory to wear face masks on public transport and in secondary schools. Similarly, in Germany, all the states have announced plans to make face masks compulsory to combat the pandemic. But several countries already face a severe shortage of PPE for their healthcare workers and patients, let alone for the healthy ones. Hence, step by step, we can expect more countries to standardise the usage of masks among the public to reduce the contamination.
Safety culture in nuclear facilities provides individual training sessions on adhering to standard procedures in Radiation Controlled Areas (RCA). The staff,
- Adhere to local rules of the workspace environment
- Avoid unnecessary touching of surfaces, the face and eyes
- Eating/drinking is prohibited within the RCA
- Protocols on careful removal of PPE
- Self-monitoring via radiation detectors and washing hands once out of an RCA
Such procedures are being recommended and implemented for the current pandemic as well to reduce transmission and surface contamination. The CDC recommends hand washing for a minimum of 20 seconds. Supermarkets have started implementing free hand-sanitizers section for customers before they enter as well as displaying signboards indicating not to touch products unnecessarily. WHO has protocols in place for handling and disposal of their masks to reduce contamination [5]. As individuals, we should also be self-aware and responsible in adhering to these protocols.
Apart from the ALARA/ALARP strategies, the nuclear industry also provides monitoring equipment (like the IPM96 Whole Body Contamination Monitor) which estimates radiation exposure rapidly and accurately for radiation workers. Such monitoring protocols have benefited the industry in managing radiation exposure to radiation workers. Also, they are useful in identifying the source of contamination quickly. Such testing procedures for SARS-CoV2 will help identify patients, clusters, effective planning, resource management and treatment. The best example in this context is Germany, who is now capable of conducting up to 500,000 tests a week. Though there are 150,000+ cases in Germany and being one of the epicentres of the pandemic, there are only 8000+ deaths, resulting in one of the lowest death rates of 4.94% (all the closed cases A/O 24 June 03, 2020) [6]. In contrast, the death rates for Italy, Spain and France are 17.27%, 15.28% and 29.47% respectively for all closed cases (A/O June 03, 2020) [6].
In conclusion, the SARS-CoV2 outbreak can take inputs from the ALARA/ALARP strategies. They include the reduction of risk of exposure based on reduced time of contact, techniques used for distance and the shielding of radiation exposure. They should be effectively utilised for developing mitigation strategies. In addition, similar protocols of rapid testing and monitoring of the SARS-CoV2 spread similar to radiation exposure can be deployed. For the current scenario, rapid testing gives us an edge in controlling the outbreak. Also, it is an interesting case to comprehend how risk assessment and mitigation strategies across various industries and technological sectors evolve from generic principles. There is always light at the end of the tunnel and we will rise together to face the crisis and solve it. However, the important factor will be the experience we will gain from handling the pandemic in the modern era. These experiences and data will be important in comprehending the loopholes in existing risk mitigation strategies, not just in the health sector but also in other domains involving risk management. Until then, stay home, stay safe.
References
- "www.worldometers.info/coronavirus/," [Online]. Available: https://www.worldometers.info/coronavirus/."
- "www.cdc.gov/nceh/radiation/alara," [Online]. Available: https://www.cdc.gov/nceh/radiation/alara.html."
- "cdc.gov/coronavirus/2019-ncov/," [Online]. Available: https://www.cdc.gov/coronavirus/2019-ncov/php/risk-assessment.html."
- "B. J. Cowling, S. T. Ali, T. W. Y. Ng, T. K. Tsang, J. C. M. Li, M. W. Fong, Q. Liao, M. Y. Kwan, S. L. Lee, S. S. Chiu, J. T. Wu, P. Wu and G. M. Leung, "Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study," The Lancet, 17 April 2020."
- "WHO. [Online]. Available: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks."
- "Johns Hopkins University Dashboard," [Online]. Available: https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6."
Author's Bio

Coming from India in 2016, Vighnesh CANDASSAMY SANTHANAMANI pursued his Masters in Nuclear Energy specialising in Nuclear Fuel Cycle at the University of Paris Saclay, France. Following, he has been part of the Assystem EOS, France, working as a design and innovation engineer since 2019. His experiences include Small Modular Reactors, Licensing, and Regulation of nuclear facilities.